I love FIGHTING fire. Nothing can be more destructive to another’s life in terms of emotion or physical pain. If someone loses their home, they may have insurance, but they will probably lose things that insurance cannot replace. Family pictures and sentimental items that mean so much to someone is can never be replaced.
I had one lady at a fire some years ago crying uncontrollably because every picture she had of her dead husband went up in flames when she lost her home. I tried to console her and I told her that probably some relative had a picture somewhere that she could make copies of. She assured me her family circle was very small and there were no other pictures. The only picture she will ever have of her dead husband is what is in her memory.
The pain of fire
Fire can also be devastating physically. The pain one endures when all or some part of their body is burning must be unspeakable. I speak of experience when I severely burned my hand some years ago when I foolishly grabbed a log on a fire that I thought was not burning in an attempt to put it deeper into the fire. The pain and blistering went on for several days as I attempted every possible means I knew of trying to diminish the pain. Of the hundreds of burn victims I have seen and dealt with over the years, nothing has affected me deeper than hearing the screams of a man who burned to death in a tractor-trailer accident one night in St. Louis because he was entangled in the wreckage. The fire was too intense to extinguish with the amount of water that was in the tank of the engine and there was no hydrant anywhere in sight to provide a water supply. By the time a second engine arrived, he had been consumed by the flames.
And of those who survive and are severely burned, the ever-lasting scars are not only physical, but emotional.
So when I say I love FIGHTING fire, it is not because I get a sense of joy or pleasure in someone else’s misery, but I see it is as an opportunity to help someone who is in need, whether it be their personal property or their life.
I also love being a paramedic and providing medical care to those in need. There is an overwhelming sense of satisfaction and joy that comes from watching someone walk out of the hospital who might have died if not for our intervention. There are the great moments also of delivering babies.
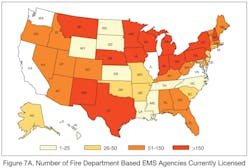
But this is what firefighter/paramedics do. In fact, that is the majority of what we do. You might say that most fire departments are really EMS agencies that sometimes go to fires. Do a breakdown of how many fires your fire department goes on and how many EMS calls your fire department goes on and you will find it is usually somewhere more than 60% EMS calls. In many fire departments, that number is probably somewhere around 90%. According to the U.S. Fire Administration (USFA), 69% of all U.S. fire departments offer emergency medical services. And as I noted in my January column (“What If the Fire Service Gets Out of EMS?”), the fire service provides EMS transports in 16 of the 20 most populous U.S. cities and provides first response to all the EMS transport providers in the other four cities.
In 2011, the United States government conducted a study called the “National EMS Assessment.” That study showed that 40% of all EMS transport agencies in the country were fire-based EMS. This study did not include all the fire departments that provide first responder service to non-fire-based EMS agencies such as third services, private ambulance companies or hospital-based EMS providers. The fire service has clearly established itself as the leading provider of EMS in the United States (see my February 2012 column, “Study Proves Fire Service Is Top EMS Provider in U.S.”).
Along with establishing yourself as the leading EMS provider, also comes the responsibility to advance the profession and shape what the future of EMS will look like. The fire service has certainly stepped up to that challenge. The International Association of Fire Chiefs (IAFC), International Association of Fire Fighters (IAFF), National Volunteer Fire Council (NVFC) and National Fire Protection Association (NFPA) all have offices or sections dedicated to EMS.
All four national fire organizations have teamed up with the Congressional Fire Service Institute (CSFI) to form the Fire Service-based EMS Advocates to ensure that Congress and the Administration more thoroughly understand the role of fire service-based EMS. Its mission is to add clarity to national policy discussions regarding EMS issues.
Ambulance standard
There are many issues facing the fire service with respect to EMS currently and in the future.
One current issue is to convince the EMS profession to accept NFPA 1917, Standard for Automotive Ambulances (see my column “NFPA 1917 Released,” November 2012). The NFPA established this technical committee after being petitioned by the IAFC. The main goal was to establish ambulance standards ensuring the safety for those who work or ride in ambulances. The current standard that many states adopted is nothing but a buying specification that the federal government issues for the purchase of ambulances. Nothing within that buying specification deals with safety.
The NFPA process of building a consensus standard is inclusive of end-users and manufacturers. In fact, only seven of the 43 principals on the NFPA 1917 technical committee came from the fire service. Unfortunately there is resistance to NFPA 1917 from some non-fire service EMS individuals. It seems you can put the word “fire” on a gold bar and these same people would somehow think the gold bar has less value.
Another issue that the fire service will have to tackle head on is how the Patient Protection and Affordable Care Act (ACA), commonly known as “Obamacare,” will impact fire service EMS in the future. The U.S. Supreme Court upheld the law in June 2011 and a Democratic president and a Democratic majority in the Senate were re-elected in November 2012, the law is bound to go into effect. Changes to the healthcare system are going to happen. Either the fire service can sit on the bus or drive the bus when it comes to how the healthcare law will impact EMS.
The ACA alone is more than 2,700 pages long and so far 14,000-plus pages of regulations have already been written. Even though EMS is rarely mentioned in the law, there will be tremendous impact on fire department EMS systems in the future. Some theorize that EMS systems will look totally different in 10 years. I do not know whether that is totally true, since there will still be people who get shot, are in car accidents and have heart attacks on the street. A system must be in place to handle those types of events. But what will be different is how we handle the chronically ill and uninsured patients that fire departments typically see, especially in urban areas.
Nobody really knows what the final picture will look like. I suspect it will always be a moving target. But what is certain is that hospitals will vie for patients who previously had no insurance, but now do. At the same time, if hospitals somehow lure those patients into their systems, they will need to carefully manage their care. The watchdog will be Accountable Care Organizations (ACOs) that will not only measure the quantity of what healthcare is delivered, but the quality of the healthcare. ACOs are affiliations of coordinated healthcare organizations that agree to be “accountable for the quality, cost and overall care of Medicare beneficiaries” assigned to them, according to the Centers for Medicare and Medicaid Services.
Under this scenario, hospitals could be penalized or not reimbursed for patients who are readmitted with the same diagnosis. For example, if a patient who was treated at a hospital with congestive heart failure is discharged, but is readmitted the next day with the same diagnosis, the hospital could be penalized or not reimbursed for the patient admission and treatment.
Thus, hospitals will need to partner with EMS systems in the future to ensure these patients are receiving the right type of care at the right facility. This may even mean an ambulance showing up at a patient’s door after a discharge from the hospital to conduct a physical assessment. I’ve heard of one hospital that is having congestive heart failure patients step on a scale each morning to measure whether they are gaining weight. The data is transmitted over the Internet to the hospital. A patient who starts gaining weight receives a visit to see what must be done to prevent readmission to the hospital. It may mean treating and releasing patients at the scene or transporting them to a facility other than a hospital.
Anticipating what a future EMS may look like, the Mesa, AZ, Fire Department has already formed a partnership with Mountain Vista Medical Center to respond to low-acuity 9-1-1 calls. A physician assistant or a nurse practitioner responds with fire department personnel to treat and release patients on the scene instead of transporting them to the hospital.
Bottom line – fire departments may not look like ambulance services in the future. Expect fire departments to form partnerships with healthcare systems. Those fire departments that do not will see private ambulance services step in to fill the void. We will still take care of those who have an acute emergency, but thing probably will change for those who are chronically ill and call 9-1-1 to go to the hospital. Thus, call volumes will drop, along with revenue since almost everyone will have insurance.
Community paramedicine
Another area that the fire service will undoubtedly have to embrace is the community paramedicine concept, which I explained in detail in my June 2012 column, “Community Paramedicine – The Next Step in EMS.” These paramedics traditionally have enhanced training and can also treat and release patients in the field. This concept is especially predicted to take hold in very rural communities where healthcare is not so readily available. Basically, the paramedic will become the only healthcare provider anywhere close. Some even feel community paramedics will be involved in dental care. Rural fire departments in the future can expect to be deeply involved in community paramedicine.
Unfortunately, when EMS came about, there was no blueprint. There was no strategic plan to follow. EMS programs developed in about six major cities with physicians training firefighters how to do medicine. Eventually, the federal government stepped in, provided legislation and funding and the rest of EMS system development has been evolutionary.
Right now, EMS is barely mentioned in the ACA and there is no dedicated funding source for EMS systems through the ACA. Additionally, there is no blueprint and no strategic plan. But somehow, fire service EMS will evolve through the process and will look different in 10 years. Fire chiefs and those who run fire service EMS programs must engage themselves in that change process; otherwise, their fire departments will be wondering what happened when they find themselves behind the curve.
For more news and training on EMS, visit http://EMSWorld.com/.