It isn’t often that a street-level medic gets the chance to prevent a medical emergency. During most shifts, we find ourselves providing medical intervention for psychiatric emergencies, motor vehicle accidents, difficulty breathing, chest pain, cardiac arrest and drug overdose.
In April 2021, the Centers for Disease Control and Prevention (CDC) and the Substance Abuse and Mental Health Services Administration said federal funding could be used to purchase fentanyl test strips (FTS). Up until then, many communities only could distribute Narcan kits without the FTS to homeless shelters, drug recovery centers, drug takeback facilities, etc.
Naloxone (Narcan nasal spray) is a safe, effective opioid overdose reversal medication. However, the inclusion of first responders in this preventative initiative has been slow to unfold.
Wisconsin’s fentanyl action
Unlike Narcan, FTS really have no place in prehospital emergency medicine. First responders deal with opioid overdoses in mostly the same ways. When we encounter depressed respiratory response, pinpoint pupils and altered mental status, we intervene with naloxone.
It makes no difference to us whether we can detect fentanyl in patients’ drugs. That takes time, which could be the difference between definitive medical care and death.
However, if we could prevent such an emergency on the front end, that would be a good thing.
In August 2022, Wisconsin Public Radio wrote that the Milwaukee County medical examiner expected record drug-related deaths in 2022. That same month, the Milwaukee Fire Department began to give out HOPE Kits, which include two FTS. The sentiment: Give first responders the opportunity to intervene before 9-1-1 is called.
Illinois’ movement
In my Illinois EMS region, training for departments that want to provide Narcan kits and FTS includes the kits and strips, to distribute to high-risk drug users.
Another avenue in Illinois is for first responders to apply to be a Drug Overdose Prevention Program (DOPP). Such organizations can order and distribute Narcan.
DOPPs are responsible for training/education, maintaining a supply of naloxone and reporting information.
Widening the scope
CDC says these programs’ concept is to lessen the crisis by equipping anybody who witnesses an opioid overdose with naloxone and the knowledge to save a life.
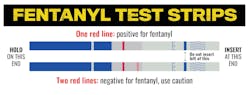
FTS, which detect the presence of fentanyl in drugs (cocaine, heroin, etc.) and drug forms (pills, powder and injectables), provide people who use drugs and communities with information about fentanyl in the illicit drug supply, so they can take steps to reduce risk of overdose.
Educating
First responders should work to educate those who use illicit drugs by emphasizing the CDC warnings:
- Keep naloxone readily available on you and at home. Talk with your healthcare provider or pharmacist about being prescribed naloxone if you or someone who you know is at risk for an overdose. Check with your health department or community organization to see whether it distributes naloxone at no cost.
- Avoid mixing drugs. Mixing stimulants (such as methamphetamine and cocaine), depressants (e.g., opioids and alcohol) or a combination can harm or kill.
- Knowing drugs’ origin doesn’t mean they’re safe, and drugs used before can produce a different reaction.
- Never use drugs alone. Make sure that people who are with you know when you took drugs in case they need to give you naloxone or call for emergency assistance.
- It’s OK to ask for help if you’re ready to get treatment for your addiction. Recovery is possible. You can find evidence-based treatment and service options near you by visiting findtreatment.gov or by calling the 24/7 National Helpline at 800-662-HELP (4357).